A diabetes reversal program is designed to help people with diabetes mellitus achieve blood sugar control and, in many cases, reverse diabetes naturally.
By targeting insulin resistance, promoting weight loss, and supporting healthy lifestyle changes, these programs aim to restore normal blood sugar levels safely and sustainably.
Unlike temporary fixes or medication-only approaches, a structured diabetes reversal plan provides personalized guidance for those with type 2 diabetes, gestational diabetes, or even patients considering bariatric surgery.
Backed by research and recommendations from authorities like the American Diabetes Association, these programs offer significant health benefits, improved energy, and long-term wellness.
How Does a Diabetes Reversal Program Work For People With Type 2 Diabetes?
A diabetes reversal program for type 2 diabetes focuses on addressing the root causes, improving blood sugar levels, and reducing reliance on diabetes medication. These programs combine dietary strategies, lifestyle changes, and medical supervision to help patients regain control over their health.
1. Weight Management and Body Composition
Excess body fat, especially excess weight or high body mass index (BMI), contributes to insulin resistance and high blood glucose. Programs encourage safe, gradual weight loss to improve insulin sensitivity and support diabetes reversal.
2. Dietary Approaches
- Low calorie diet (LCD): Helps reduce overall calorie intake to support weight loss and stabilize blood sugar levels.
- Very low calorie diet (VLCD): Used under medical supervision for rapid results in select patients, often leading to significant improvements in insulin sensitivity.
3. Medication Adjustment
Structured programs monitor diabetes medication usage closely. As blood glucose stabilizes through diet, exercise, and lifestyle changes, some patients may gradually reduce or stop certain medications under supervision.
4. Prevention of Complications
By controlling blood sugar levels and managing excess weight, programs reduce risks of kidney disease, cardiovascular issues, and other diabetes-related complications.
5. Early Intervention for High-Risk Individuals
For people at risk who may develop diabetes, programs focus on early lifestyle changes, improving diet and physical activity, and preventing disease progression.
Can Lifestyle Changes Lead To Long-Term Diabetes Reversal Without Medications?
Yes. For many people with type 2 diabetes, structured lifestyle changes can help achieve diabetes remission without relying solely on medications. By addressing high blood sugar, promoting safe weight loss, and improving overall metabolic health, patients can regain better control of their condition.
While some obese patients may benefit from metabolic surgery or gastric bypass, many can improve insulin production naturally through diet, exercise, and stress management. These changes also support mental health, cardiovascular protection, and overall disease control.
Key Lifestyle Strategies:
- Lose Weight Safely: Reducing excess body weight improves insulin sensitivity and helps normalize blood sugar levels.
- Balanced Diet: Focus on whole foods, low-glycemic carbohydrates, lean protein, and healthy fats to support producing insulin efficiently.
- Regular Physical Activity: Aerobic and resistance exercises enhance insulin production and help maintain long-term disease control.
- Stress Management & Mental Health: Reducing stress supports hormone balance, which is critical in managing diabetes effectively.
- Monitoring & Consistency: Regular tracking of blood sugar and consistent habits are essential for maintaining diabetes remission.
What Natural Methods Help Stabilize Blood Sugar Effectively?
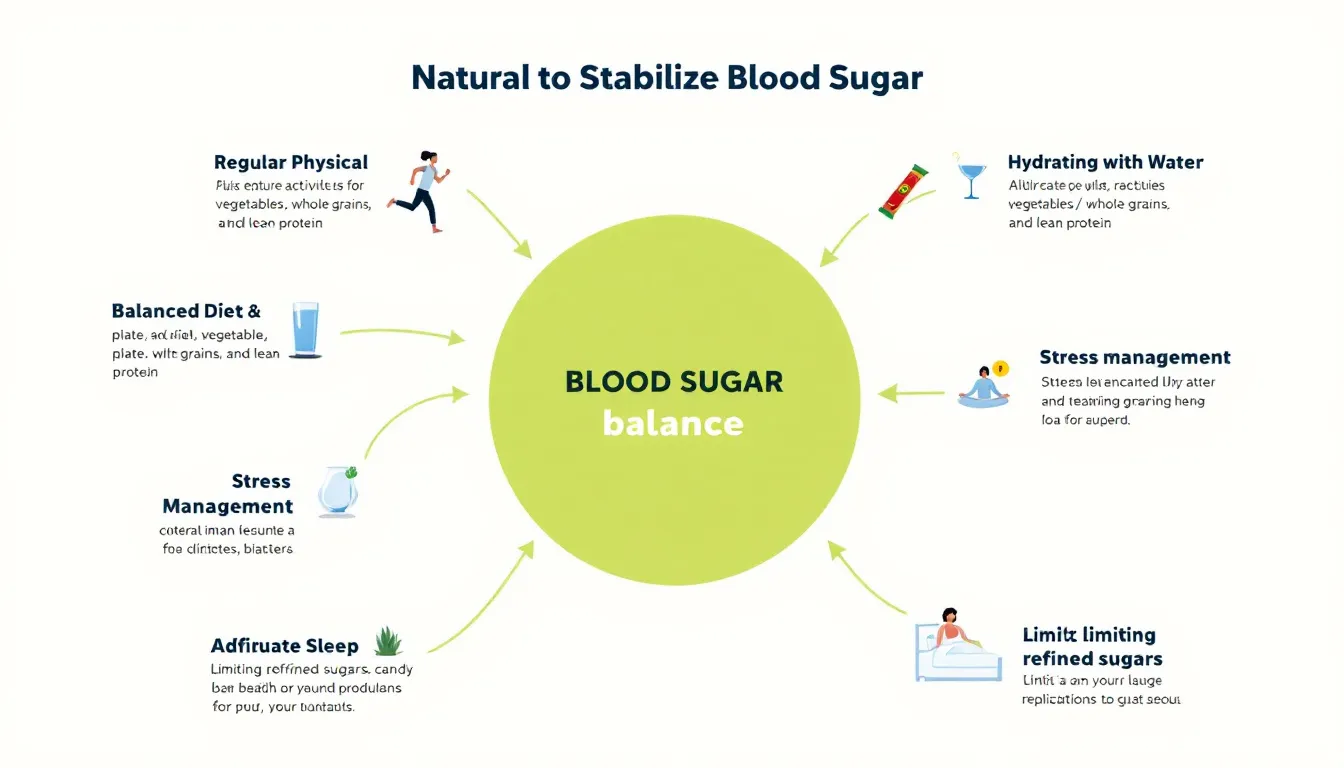
Stabilizing blood sugar naturally is key to long-term diabetes management, improving insulin levels, and supporting beta cell health. Combining diet, exercise, and lifestyle adjustments can help maintain optimal sugar levels over an extended period and reduce the need for taking insulin in some patients.
1. Dietary Changes for Blood Sugar Control
Dietary changes are central to stabilizing blood sugar.
- Choose low-glycemic foods like brown rice, whole grains, vegetables, and legumes to prevent sugar spikes.
- Prioritize balanced diet with protein, fiber, and healthy fats to optimize insulin levels and improve beta cells function.
- Avoid refined sugars and processed foods, which can overload the pancreas and reduce enough insulin production.
2. Regular Exercise
Regular exercise enhances insulin sensitivity, allowing the body to use insulin more efficiently.
- Both aerobic and resistance training help stabilize blood glucose.
- Exercise is particularly beneficial for obese people, improving metabolic health and reducing diabetes risk over time.
- Consistent activity over an extended period promotes long-term control of blood sugar levels.
3. Supporting Beta Cell Health
Healthy beta cells are essential for proper insulin secretion.
- Adequate nutrition, exercise, and stress management support beta cells and help maintain enough insulin for glucose regulation.
- Avoiding chronic high sugar intake prevents exhaustion of beta cells, especially in young age or early-stage type 2 diabetes.
4. Monitoring and Assessment
Tracking progress helps guide natural interventions.
- Longitudinal assessment of sugar levels ensures the program is effective over time.
- Regular monitoring can reduce dependence on taking insulin in controlled cases and inform dietary or exercise adjustments.
5. Additional Considerations
- For obese people, combining diet and exercise may sometimes prevent the need for laparoscopic sleeve gastrectomy or other metabolic surgery.
- Research like aging studies highlights that lifestyle changes can preserve beta cell function and maintain optimal insulin levels even with advancing age.
How Is Diabetes Mellitus Treated Through Lifestyle And Medical Interventions?
Diabetes mellitus, particularly type 2 diabetes, is a chronic condition characterized by impaired glycemic control, often influenced by genetic predisposition and lifestyle factors such as excess fat accumulation.
Treatment requires a combination of lifestyle modifications and medical interventions aimed at improving insulin sensitivity, reducing blood sugar levels, and preventing long-term health concerns.
1. Lifestyle Modifications
Lifestyle interventions are the first line of treatment for managing type 2 diabetes and improving overall metabolic health:
- Dietary Adjustments:
- Emphasize whole grains for slow-digesting carbohydrates.
- Increase intake of non-starchy vegetables to boost fiber and stabilize blood sugar.
- Reduce intake of refined sugars, saturated fats, and processed foods that contribute to excess fat and poor glycemic control.
- Weight Management:
- Achieving a healthy weight through lifestyle modifications significantly improves insulin sensitivity.
- Even modest weight loss can reduce reliance on medications and lower risk of complications.
- Physical Activity:
- Regular aerobic exercise and resistance training enhance insulin sensitivity and improve glycemic control.
- Encourages fat loss, particularly visceral fat, which is strongly linked to insulin resistance.
- Stress Management & Sleep:
- Chronic stress and poor sleep can elevate blood sugar and worsen type 2 diabetes.
- Mindfulness, meditation, and consistent sleep routines support overall health and blood sugar regulation.
2. Medical Interventions
When lifestyle changes alone are insufficient, medical interventions are considered:
- Oral Medications and Insulin Therapy:
- Drugs like metformin, SGLT2 inhibitors, or GLP-1 agonists help improve glycemic control.
- Some patients may require taking insulin to maintain normal glucose levels.
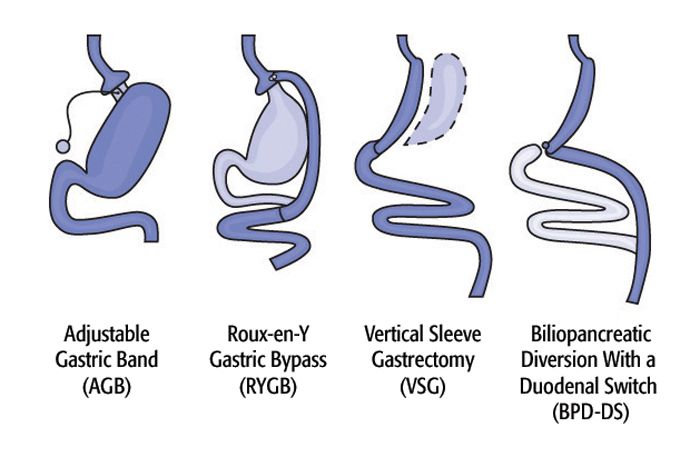
- Bariatric Surgery:
- For obese patients or those with uncontrolled type 2 diabetes, procedures like laparoscopic gastric bypass, gastric banding, or other surgical approaches may be recommended.
- Studies, including bariatric surgery studies, show these surgeries can significantly improve blood sugar levels and even induce remission in some cases.
- Regular Monitoring:
- Continuous monitoring of glycemic control, kidney function, and cardiovascular health ensures long-term management and helps prevent complications.
3. Integrated Approach
Optimal treatment for diabetes mellitus combines lifestyle modifications with medical interventions tailored to individual risk factors, genetic predisposition, and metabolic status.
- Early intervention improves glycemic control, reduces medication dependence, and promotes overall health.
- Coordinated care addresses health concerns like heart disease, kidney disease, and nerve complications while supporting long-term disease management.
What Is Gestational Diabetes And How Can It Be Managed Safely?

Gestational diabetes (GDM) is a condition characterized by high blood sugar levels that develop during pregnancy, usually in the second or third trimester.
It occurs when the body cannot produce enough insulin to meet the increased demands of pregnancy, leading to weight gain and elevated glucose levels. While temporary in most cases, proper management is crucial to prevent complications for both mother and baby.
Unlike type 2 diabetes, there is no permanent cure, but careful strategies can control blood sugar effectively.
1. Understanding Gestational Diabetes
- Cause: Hormonal changes during pregnancy can lead to insulin resistance, making it harder for the body to use insulin efficiently.
- Risk Factors: Includes weight gain during pregnancy, previous history of gestational diabetes, family history of diabetes, or obesity.
- Complications if Unmanaged: Poorly controlled GDM increases the risk of preeclampsia, macrosomia (large babies), and may impact long-term metabolic health of both mother and child.
2. Lifestyle Management
Lifestyle interventions are the first line of management:
- Dietary Adjustments:
- Implement calorie restriction with nutrient-dense foods to maintain healthy blood sugar levels.
- Emphasize whole grains, lean protein, fruits, vegetables, and healthy fats.
- Avoid refined sugars and processed foods to prevent spikes in blood glucose.
- Weight Monitoring:
- Healthy weight gain during pregnancy is essential; excessive gain worsens insulin resistance.
- Regular check-ups help ensure weight gain is within recommended limits.
- Physical Activity:
- Moderate exercise, approved by an obstetrician, can improve insulin sensitivity.
- Activities like walking, prenatal yoga, or light strength training are beneficial.
3. Medical Management
For some women, lifestyle measures alone may not suffice, and medical interventions are needed:
- Medication: Insulin therapy may be prescribed if blood sugar cannot be controlled with diet and exercise.
- Monitoring: Frequent glucose checks ensure optimal glycemic control and prevent complications.
- Internal Medicine Consultation: Collaboration with specialists in internal medicine or endocrinology ensures individualized care for both mother and baby.
4. Special Considerations
- Bariatric Surgery History: Women with previous gastric sleeve or other metabolic surgeries may require tailored monitoring due to altered nutrient absorption.
- Long-Term Health: While GDM often resolves postpartum, women remain at higher risk for type 2 diabetes, so postnatal follow-up is critical.
Is Bariatric Surgery a Permanent Solution For Diabetes Reversal?
Bariatric surgery is increasingly recognized as a highly effective intervention for people with diabetes, particularly type 2 diabetes, who struggle with obesity or poor glycemic control.
However, it is important to understand that while it can lead to diabetes remission, it is not necessarily a permanent cure, and ongoing lifestyle management remains essential.
1. Understanding Bariatric Surgery and Its Effects on Diabetes
Bariatric procedures, such as gastric sleeve or gastric bypass, work primarily by:
- Reducing stomach size, which limits food intake and encourages patients to eat smaller portions.
- Altering gut hormones to improve insulin sensitivity and glycemic control.
- Supporting rapid weight loss, which plays a crucial role in lowering blood sugar levels.
Clinical studies show that many patients experience diabetes remission within months of surgery, often allowing a reduction or complete cessation of diabetes medications.
2. Why Bariatric Surgery Is Not Always a Permanent Solution
While the results of bariatric surgery are promising, it is important to note:
- Surgery addresses the symptoms and metabolic dysfunction but does not always define cure. Long-term success depends on sustained lifestyle changes.
- Patients must adhere to dietary guidelines, including a diet low in refined sugars and processed foods.
- Regular monitoring is needed, especially in pregnant women, as nutritional demands change and blood sugar must be carefully managed.
- Weight regain or poor adherence to post-surgery habits can lead to recurrence of diabetes.
3. Role of Lifestyle and Ongoing Support
- Dietary Management: Post-surgery, patients are advised to eat nutrient-dense meals, eat smaller portions, and follow balanced diets to maintain glycemic control.
- Exercise: Physical activity remains essential for maintaining weight loss and insulin sensitivity.
- Monitoring: Regular follow-up with healthcare providers ensures early detection if blood sugar rises again.
4. Research and Long-Term Outcomes
- Ongoing research indicates that bariatric surgery can induce long-term remission in many patients, but outcomes vary based on age, duration of diabetes, obesity level, and adherence to lifestyle modifications.
- Studies suggest that combining surgery with structured lifestyle support has the highest probability of sustained diabetes reversal.
What Factors Increase The Risk To Develop Diabetes In Adults?

Diabetes, especially type 2 diabetes, is a chronic metabolic disorder characterized by high blood sugar levels caused by insulin resistance or impaired insulin secretion.
A significant number of adults worldwide are at risk due to a combination of genetic, lifestyle, and environmental factors. Understanding these risk factors is crucial for prevention, early detection, and management.
1. Genetic Predisposition and Family History
- Adults with a family history of diabetes have a higher likelihood of developing the condition.
- A significant number of people inherit genes that influence insulin production, beta cell function, or fat distribution, increasing susceptibility.
- Genetic predisposition alone does not guarantee diabetes, but it amplifies risk when combined with lifestyle factors.
2. Obesity and Excess Body Fat
- Excess fat, particularly visceral fat around the abdomen, contributes to insulin resistance.
- Obesity is one of the strongest predictors for type 2 diabetes, affecting blood sugar control.
- A significant number of adults with obesity eventually develop diabetes if no preventive measures are taken.
3. Sedentary Lifestyle
- Lack of physical activity reduces insulin sensitivity and promotes weight gain.
- Sedentary behavior, including prolonged sitting at work or home, is linked to poor glycemic control.
- Adults with minimal exercise have a significant risk of developing diabetes over time.
4. Unhealthy Diet and Nutritional Factors
- Diets high in refined sugars, processed foods, and unhealthy fats increase the risk of diabetes.
- Insufficient intake of whole grains, fiber, and vegetables affects blood sugar regulation.
- Calorie-dense diets contribute to weight gain and insulin resistance, affecting a significant number of adults.
5. Age and Metabolic Changes
- The risk of diabetes rises with age, particularly after 40, due to declining insulin production and changes in metabolism.
- Aging is associated with increased fat accumulation and reduced muscle mass, both of which impact blood sugar control.
6. Medical Conditions and Hormonal Factors
- Conditions such as hypertension, polycystic ovary syndrome (PCOS), and dyslipidemia increase the risk of diabetes.
- Adults who have had gestational diabetes are more likely to develop type 2 diabetes later in life.
- A significant number of adults with metabolic syndrome exhibit these risk factors simultaneously.
7. Environmental and Socioeconomic Factors
- Urbanization, stress, lack of access to healthy foods, and socioeconomic challenges contribute to diabetes risk.
- Exposure to endocrine-disrupting chemicals and chronic stress can impair insulin sensitivity in a significant number of adults.
8. Lifestyle Habits and Smoking
- Smoking and excessive alcohol consumption impair beta cell function and glycemic control.
- Adults with these habits have a significant likelihood of developing type 2 diabetes compared to non-smokers or moderate drinkers.
9. Sleep and Mental Health
- Chronic sleep deprivation and untreated mental health conditions, like depression, negatively affect blood sugar regulation.
- Poor sleep patterns increase cortisol levels, promoting insulin resistance, which puts a significant number of adults at risk.
What Is Diabetes Reversal Program? HealthyWayFit — India’s Most Personal Clinic-Based Solution

Living with diabetes often feels like carrying an invisible weight. You’re told to “eat less,” “exercise more,” or “try another pill.” Yet your blood sugar stays stubborn, energy dips continue, and every lab report feels like a warning. The missing piece isn’t willpower — it’s a structured diabetes reversal program guided by experts.
That’s where HealthyWayFit’s Diabetes Reversal Clinic comes in.
We are not another app, generic webinar, or mass-market diet chart. HealthyWayFit offers a 12-month, doctor-led, end-to-end diabetes reversal program designed specifically for Indian professionals who want a clinic-based system tailored to their lifestyle.
Over the years, our diabetes specialists have guided hundreds of patients toward lowering HbA1c, reducing medication dependency, and — in many cases — achieving complete diabetes reversal.
Our approach is simple: empathetic, therapeutic, and committed. We listen first, design second, and stay with you throughout your diabetes reversal program journey.
1) What Makes HealthyWayFit’s Diabetes Reversal Program Different?
1. Doctor-Led Personalized Nutrition
No quinoa fads or complicated smoothie charts. Our doctors and nutritionists integrate your ghar ka khana — dal, roti, rice, idli, dosa, paneer, sabzi — with your blood sugar control. A practical plan you can follow at 35 or 85.
2. Metabolic Exercise That Works Fast
Simple metabolic movements targeting major muscle groups (legs, shoulders, glutes) take just 15–20 minutes daily and can reduce sugar levels by 50–100 points. No gym needed.
3. Stress & Sleep Mastery
Stress raises cortisol, which spikes blood sugar. Our clinic specialists teach one-minute breathing routines, sleep optimization, and micro-habits to stabilize sugars even during busy schedules.
4. Holistic, Doctor-Led Care
Work directly with a Senior MD Diabetologist who monitors your medical safety while lifestyle coaches optimize habits. This blend of medical oversight and lifestyle expertise ensures your diabetes reversal program works effectively.
5. Relentless Support & Accountability
Weekly coaching calls, daily check-ins, habit tracking, and practical guides for festivals, dining out, travel, and weddings. Life won’t stop — and neither will your program.
2) What Results Can You Expect?
Most patients notice improvements in 20–60 days: better energy, lighter mornings, and lower sugar readings. Over the full diabetes reversal program, results are sustainable, not temporary, year after year.
3) Is This Diabetes Reversal Program for You?
If you are a working professional or entrepreneur serious about taking control of your diabetes and can dedicate 15–30 minutes a day, this clinic-based diabetes reversal program is ideal. It’s not a crash course — it’s a life-changing system built around your food, family, and lifestyle.
4) Take the Next Step
Your journey begins with a personal consultation at our diabetes reversal clinic, where we understand your current health markers, challenges, and lifestyle. Once aligned, we design a custom doctor-led diabetes reversal program just for you.
Visit HealthyWayFit to explore how you can move beyond “managing” diabetes and actually reverse diabetes — sustainably, safely, and with expert supervision.
Book your consultation directly here: Calendly Appointment
Frequently Asked Questions(FAQs)

1. What daily habits should diabetic patients adopt to improve health?
Diabetic patients should focus on consistent healthy eating, regular physical activity, stress management, adequate sleep, and monitoring blood sugar levels. Drinking enough water, limiting processed foods, and following medication advice are crucial.
Daily habits supporting weight management and balanced nutrition improve overall health and reduce complications.
2. What steps can lead to diabetes remission naturally?
Diabetes remission can be supported through weight loss, a balanced low-calorie diet, regular exercise, and stress management. Limiting refined sugars, increasing fiber, and adopting sustainable lifestyle modifications improve insulin sensitivity.
Early intervention, consistent habits, and professional guidance can help some patients achieve partial or full remission naturally.
3. How does genetic predisposition affect diabetes risk?
Genetic predisposition increases the likelihood of developing type 2 diabetes. Individuals with family history of diabetes may inherit traits affecting insulin production, beta cell function, or fat metabolism.
While genes play a role, lifestyle factors like diet, activity, and weight also influence whether a genetically predisposed person develops diabetes.
4. What role do beta cells play in diabetes?
Beta cells, located in the pancreas, produce insulin, which regulates blood sugar levels. Dysfunction or destruction of beta cells reduces insulin production, leading to hyperglycemia.
In type 1 diabetes, autoimmune attack destroys beta cells, while in type 2, beta cells gradually fail under insulin resistance, contributing to chronic diabetes.
5. What is the most common form of diabetes and its symptoms?
Type 2 diabetes is the most common form, often developing in adults but increasingly seen in younger populations. Symptoms include frequent urination, excessive thirst, fatigue, blurred vision, slow-healing wounds, and increased hunger.
Insulin resistance and gradual beta cell dysfunction characterize its progression, often linked to obesity and sedentary lifestyle.
Conclusion
A structured diabetes reversal program offers more than symptom management—it addresses the root causes of diabetes by improving insulin sensitivity, supporting weight management, and restoring normal blood sugar levels.
Unlike temporary solutions, it combines doctor-led care, lifestyle modifications, and ongoing support, making reversal both safe and sustainable. For many, this means reduced medications, better energy, and protection from long-term complications.
Whether dealing with type 2 diabetes, gestational diabetes, or considering advanced interventions like bariatric surgery, the right program empowers individuals to move beyond control toward lasting health and true transformation in their diabetes journey.

.jpg)
