Many people wonder if it’s truly possible to reverse diabetes, and research shows that in many cases, it is achievable through consistent lifestyle changes. The journey of reversing diabetes often begins with small steps like improving diet, building regular exercise habits, and focusing on gradual weight loss.
These changes not only help in better blood sugar control but also reduce insulin resistance, one of the root causes of type 2 diabetes.
When the body becomes more sensitive to insulin, it’s easier to maintain normal blood sugar levels, which lowers the risk of complications and boosts energy naturally. By taking proactive steps, individuals can move closer to long-term health and improved quality of life.
Is diabetes reversal possible through lifestyle changes or medical treatment?

Yes, in many cases, diabetes reversal is possible through both lifestyle changes and medical interventions.
While diabetes is often seen as a chronic disease, studies show that individuals can reverse diabetes by targeting the root causes such as insulin resistance, excess weight, and consistently high blood sugar levels.
The American Diabetes Association recognizes that sustained changes like a low calorie diet, bariatric surgery, or structured medical care can lead to significant improvements.
For some, especially those with gestational diabetes, early lifestyle intervention may prevent progression to type 2 diabetes. The key lies in improving blood sugar control, reducing insulin resistance, and achieving normal blood sugar levels through healthy, long-term habits.
Ways to Support Diabetes Reversal:
- Adopt lifestyle changes – Regular exercise and balanced nutrition help in reversing diabetes and improving blood glucose levels.
- Lose weight safely – Reducing body mass index through gradual weight loss supports better blood sugar management.
- Low calorie or very low calorie diet – Research shows these diets may trigger diabetes reversal in some patients.
- Improve insulin sensitivity – Reducing insulin resistance allows the body to process glucose more effectively.
- Medical treatments – Options like bariatric surgery offer significant health benefits by improving blood sugar levels in obese patients.
- Monitor regularly – Keeping track of blood sugar and preventing high blood sugar spikes ensures sustainable results in reversing diabetes.
What is insulin resistance and how does it impact overall health?
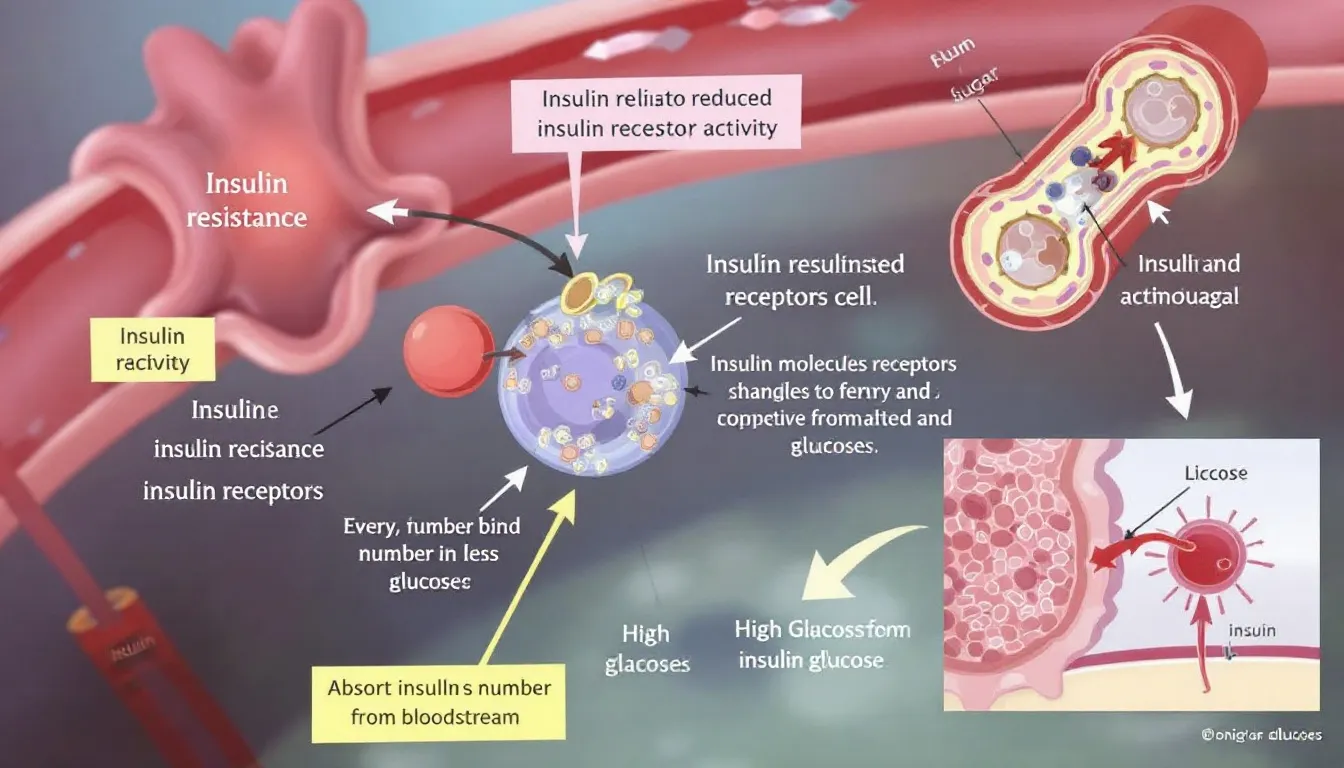
Insulin resistance happens when the body’s cells don’t respond effectively to insulin, causing higher insulin levels and elevated blood sugar. Over time, this puts pressure on the beta cells in the pancreas, which must work harder to produce more insulin.
If unmanaged, it can lead to diabetes, weight gain, and related complications. According to experts in internal medicine, insulin resistance is one of the earliest red flags that needs careful attention to prevent diabetes.
While there is no magic pill or quick define cure, lifestyle strategies such as a diet low in processed foods, engaging in regular physical activity, and learning to eat smaller portions can help.
Insulin resistance also impacts overall health by increasing the risk of heart disease, fatty liver, and conditions like sleep apnea.
For pregnant women, insulin resistance may contribute to gestational diabetes, which requires careful monitoring as part of diabetes care. For those recently diagnosed, early action and ongoing research into treatment approaches provide hope for better management.
Key Impacts of Insulin Resistance on Health:
- Strains the pancreas and damages beta cells, increasing the likelihood of type 2 diabetes.
- Raises blood sugar and may progress from prediabetes to diabetes if not addressed.
- Contributes to weight gain and complicates efforts to prevent diabetes.
- Increases risks of cardiovascular disease, fatty liver, and sleep apnea.
- Can complicate pregnancies in pregnant women, often requiring specialized diabetes care.
- Highlights the need for lifestyle changes—physical activity, a diet low in refined carbs, and strategies like eat smaller portions.
In short, managing insulin resistance through healthy habits and medical guidance is the most effective way to reduce risk and support long-term health.
Can gestational diabetes increase the risk of type 2 diabetes later in life?
Gestational diabetes significantly raises the risk of developing type 2 diabetes later in life. While many women see their blood sugar return to a normal range after delivery, research shows that a history of gestational diabetes often leaves them more vulnerable.
In fact, studies in diabetes mellitus highlight that women with this condition are several times more likely to be diagnosed with type 2 diabetes compared to those who never had it.
The risk is even higher for obese patients, as excess weight makes insulin resistance worse and complicates long-term glucose management.
1) Health Concerns Linked to Gestational Diabetes
If unmanaged, gestational diabetes may contribute to recurring diabetes symptoms and broader health concerns. Poor control over blood sugar not only increases the chance of developing type 2 diabetes but can also affect kidney function, sometimes leading to kidney disease in the long term.
For women with additional risk factors such as obesity or family history, this progression can be even faster without intervention.
2) Role of Lifestyle Changes and Diet
The good news is that lifestyle changes can greatly reduce the risks. A diet that focuses on fiber-rich foods and whole grains, combined with moderate calorie restriction, helps regulate blood sugar more effectively.
Women who commit to steady and sustainable weight management often achieve better outcomes, as even small amounts of achieved weight loss are linked to reduced diabetes risk. Incorporating regular exercise and dietary changes makes it easier to maintain balance and prevent future complications.
3) Medical Monitoring and Interventions
Regular blood tests are important for detecting changes in glucose before serious diabetes symptoms develop. In some cases, especially for those with higher BMI, medical procedures such as gastric bypass or gastric sleeve surgery may be recommended.
These interventions, combined with healthy habits, can help reduce the likelihood of transitioning from gestational diabetes to type 2 diabetes.
How effective is bariatric surgery in managing or reversing diabetes?
1) Bariatric Surgery and Its Role in Disease Control
Bariatric surgery, also known as metabolic surgery, has emerged as one of the most effective treatments for managing diabetes and, in many cases, achieving diabetes remission.
Unlike standard lifestyle or medication-based approaches, surgery directly addresses the underlying cause of type 2 diabetes by targeting excess fat, which is strongly linked to insulin resistance and poor blood sugar regulation.
For many patients, bariatric surgery offers not just weight reduction but also significant improvements in disease control.
2) Impact on Insulin Sensitivity and Insulin Production
One of the primary ways bariatric surgery helps is by improving insulin sensitivity. When the body sheds excess fat, cells become more responsive to insulin, making it easier to maintain normal blood sugar levels.
In addition, the procedure often stimulates changes in the gut and hormones that enhance insulin production from the pancreas. This improved ability to process glucose reduces the strain on beta cells responsible for producing insulin, slowing down the progression of type 2 diabetes.
3) Achieving Diabetes Remission
Research shows that a significant percentage of patients undergoing bariatric or metabolic surgery experience partial or complete diabetes remission. In some cases, blood sugar normalizes within days of surgery, even before major weight loss occurs.
This rapid change is linked to hormonal adjustments in the digestive system that regulate appetite, glucose absorption, and insulin action. However, long-term remission depends on maintaining a healthy lifestyle post-surgery, as diabetes can return if unhealthy habits resurface.
4) Benefits Beyond Blood Sugar Control
The advantages of bariatric surgery extend beyond glucose management. Patients often see improvements in cardiovascular health, lower cholesterol levels, reduced blood pressure, and enhanced overall metabolic function.
The reduction in excess fat helps alleviate stress on multiple organs, supporting better outcomes for long-term disease control.
For many individuals, surgery not only improves the ability to live without constant medication but also reduces the risk of complications commonly associated with uncontrolled diabetes.
5) Long-Term Effectiveness and Considerations
While bariatric surgery is highly effective, its success depends on patient commitment. Long-term diabetes remission requires consistent follow-up care, balanced nutrition, and physical activity. Without these, blood sugar problems can reappear.
Patients must also be aware that surgery carries risks and is generally recommended for individuals with severe obesity or those who have not achieved results through conventional methods.
What are the early warning signs and common diabetes symptoms to watch for?

1) Early Signs of Diabetes
Diabetes begins quietly, and many people don’t notice the earliest warning signs. When the body is not making enough insulin or cannot use insulin properly, glucose builds up in the bloodstream.
This leads to high blood sugars, which cause classic symptoms such as excessive thirst, frequent urination, extreme hunger, and unusual fatigue. Some people may also experience sudden, unexplained weight changes.
At this stage, poor glycemic control is already affecting the body, even if the symptoms feel mild. Recognizing these early signs is important because timely intervention can slow or even prevent disease progression.
2) Common Diabetes Symptoms
As blood sugars remain uncontrolled, additional diabetes symptoms appear. Many individuals notice blurred vision due to fluid changes in the eyes, slow-healing wounds caused by impaired circulation, and tingling or numbness in hands and feet, which indicate nerve involvement.
Recurring infections, such as urinary tract or skin infections, are also common because elevated glucose creates an environment favorable for bacteria.
These symptoms highlight that the body is struggling to achieve stable glycemic control, and professional diabetes care becomes necessary at this point.
3) Role of Diet and Lifestyle in Symptom Management
Nutrition and lifestyle play a central role in managing and reducing diabetes symptoms. A balanced diet that emphasizes non starchy vegetables, fiber, and healthy fats supports better regulation of blood sugars.
Avocados, nuts, olive oil, and seeds improve satiety and insulin response, while avoiding excess refined carbs helps limit spikes. Portion control and regular physical activity further contribute to maintaining glycemic balance.
With consistent habits, people can improve their overall glycemic control, reduce complications, and feel more energetic day to day.
4) Can Diabetes Be Reversed?
An important question many ask is: Can diabetes be reversed? Research shows that in certain cases, especially for those with obesity, remission is possible.
Every major bariatric surgery study demonstrates that procedures like laparoscopic gastric bypass and gastric banding can significantly improve insulin sensitivity and sometimes restore normal glucose metabolism.
These surgeries help reduce excess weight, improve hormone balance, and in some cases lead to full diabetes remission.
However, success depends on more than surgery alone—it requires lifelong dietary adjustments, exercise, and regular monitoring. While not everyone achieves reversal, many patients experience dramatic improvements in glycemic control and overall health.
How can someone develop diabetes even with a healthy lifestyle?

1) Genetic and Biological Predisposition
Even people who follow healthy diets and exercise regularly may develop type 2 diabetes because genetics play a powerful role. If someone has a family history of diabetes, their body may naturally have reduced insulin efficiency or fewer functioning beta cells.
This means that even with a balanced diet and normal body weight, blood sugar levels may rise over time. Aging also reduces insulin sensitivity, making it harder to keep blood sugar stable.
In such cases, lifestyle cannot completely offset the inherited risk, and diabetes may appear as a chronic disease despite healthy living.
2) The Role of Stress, Hormones, and Sleep
Many people underestimate how much stress and hormones affect metabolism. High stress increases cortisol, a hormone that raises blood sugar. Similarly, sleep deprivation or disorders like sleep apnea can worsen insulin resistance, leading to elevated blood sugar levels.
Women with hormonal conditions such as PCOS are also more likely to develop type 2 diabetes even if they are not overweight. These factors prove that diabetes is not always caused by overeating or inactivity—it can emerge from hidden internal imbalances.
3) Environmental and Lifestyle Influences Beyond Diet
Even a “healthy lifestyle” may not always be enough if environmental factors interfere. For instance, prolonged exposure to pollutants, sedentary desk jobs despite daily exercise, or consuming foods thought to be “healthy” but high in hidden sugars can still affect blood sugar control.
Additionally, certain medical treatments or long-term medication use can disrupt glucose regulation, pushing otherwise healthy individuals toward diabetes.
4) Why Some Normal-Weight People Develop Diabetes
A common misconception is that diabetes only affects those who are overweight. In reality, even people with normal or low body mass index can develop type 2 diabetes. This happens because the body may store fat around organs (visceral fat) even if it is not visible externally.
This type of fat interferes with insulin sensitivity, causing high blood sugar. For such individuals, lifestyle measures alone may not prevent diabetes, and they might require medical monitoring or diabetes medications to manage their condition.
5) The Possibility of Reversing Diabetes
While not everyone can completely reverse diabetes, many people can achieve significant improvement or remission. Intensive weight loss programs, structured diets, and increased activity have been shown to lower blood sugar levels and improve insulin sensitivity.
Clinical studies highlight that reversing diabetes often requires consistent and long-term effort, focusing on reducing blood sugar spikes and protecting pancreatic function.
Some individuals may succeed through nutrition and exercise alone, while others need support from diabetes medications or medical procedures. The goal is always better blood sugar control, fewer complications, and improved quality of life.
What is the difference between diabetes remission and complete cure?
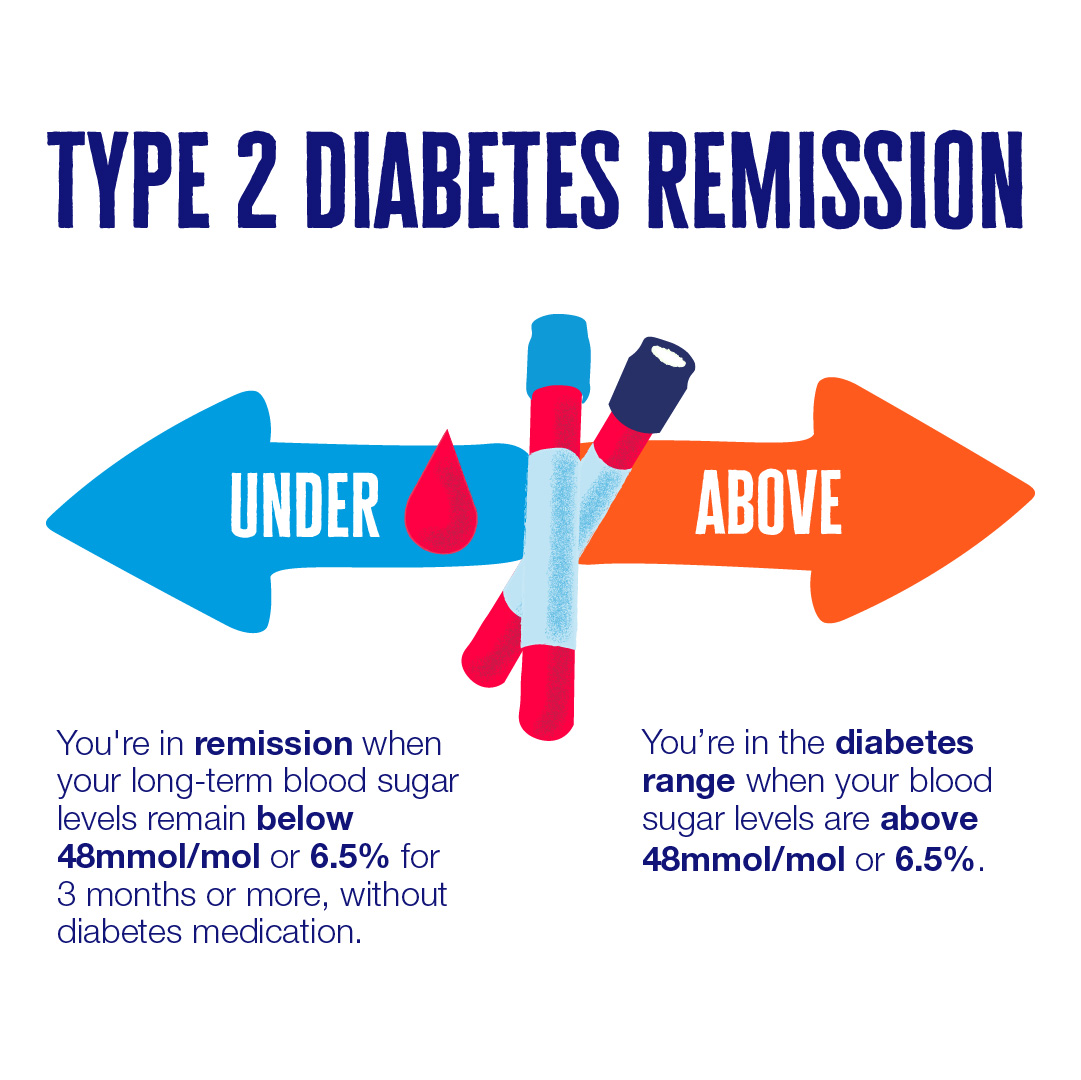
1. Understanding Diabetes Remission
Diabetes remission happens when a person’s blood sugar levels return to the normal range without the need for ongoing medication.
For many diabetic patients, this state can be achieved through lifestyle changes such as weight loss, following a very low calorie diet, or adopting healthier eating patterns rich in healthy fats and whole foods.
Remission doesn’t mean the condition is gone forever—it simply means it is under control at the moment. Factors like stress, poor diet, or regaining weight can trigger high blood sugar again, showing that remission requires long-term commitment.
2. Why Diabetes Is Not Considered Completely Cured
Unlike some infections that disappear entirely, diabetes is a chronic condition, and experts hesitate to use the word “cure.” Even if someone manages to reverse diabetes and maintain normal glucose without medications, the underlying susceptibility remains.
For instance, if a person regains weight or stops following their healthy routine, their risk of developing high blood sugar returns. This is why doctors describe the condition as “in remission” rather than “cured.”
A true cure would mean the risk of diabetes is permanently gone—which current science cannot guarantee.
3. The Role of Lifestyle in Achieving Remission
Lifestyle changes are the most powerful tools to help reverse diabetes and achieve remission. Significant weight loss, especially in the early stages, has been shown to restore the body’s insulin sensitivity and reduce the strain on the pancreas.
Some people benefit from structured approaches such as a very low calorie diet, which lowers fat around the liver and pancreas. Adding healthy fats like avocado, nuts, and olive oil, along with balanced exercise, supports steady blood sugar control while also improving blood pressure and heart health.
4. Key Difference Between Remission and Cure
The difference is subtle but crucial:
- Remission means diabetes is controlled without medications, but the risk of relapse remains.
- Cure would mean the disease is gone permanently with no chance of returning.
Currently, the medical consensus is that people can achieve remission through weight loss, diet, and lifestyle, but not a guaranteed cure. For now, diabetic patients are encouraged to focus on long-term strategies to manage and maintain remission rather than expecting a permanent cure.
Is Diabetes Reversal Possible? A Look at Leading Programs in India

Many people ask: “Is diabetes reversal possible, or is it only about lifelong management?” The rise of specialized reversal programs in India shows that, with the right approach, it can be achieved. Let’s look at how three leading brands are making diabetes reversal a reality.
Sugarfit
Background:
Founded in 2021 in Bengaluru, Sugarfit is a health-tech startup that focuses on type 2 diabetes and pre-diabetes reversal. Instead of relying on long-term medication, Sugarfit empowers individuals through data-driven lifestyle changes.
Philosophy:
Sugarfit believes diabetes reversal is possible when care is personalized, preventive, and guided by real-time health data.
How It Works:
- Continuous Glucose Monitoring (CGM): Tracks daily glucose variations, helping users understand their food and activity impact.
- Medical Oversight: Doctors monitor progress and adjust medications as blood sugar improves.
- Personalized Nutrition & Fitness: Plans built around Indian meals and individual glucose responses.
- Stress & Mindfulness: Breathing, meditation, and behavioral coaching for sugar stability.
- Community & Lab Tracking: Screenings and support through live sessions.
Outcomes:
- Participants with HbA1c >9 have seen ~20% reduction in 90 days.
- Many taper off or stop medicines.
- Users report more energy, improved sleep, and better weight control.
Positioning:
For digitally literate urban patients who want evidence that diabetes reversal is possible using tech-enabled, structured care.
Twin Health
Background:
Silicon Valley-founded Twin Health brought its Whole Body Digital Twin™ (WBDT™) to India, offering AI-driven metabolic care through hospitals and corporate tie-ups.
Philosophy:
Diabetes isn’t just high sugar; it’s a result of systemic metabolic imbalances. Twin Health aims to show that reversal is possible by fixing these root causes.
How It Works:
- Whole Body Digital Twin™: Creates an AI-based digital model of each individual’s metabolism.
- Wearables & Tracking: CGM, activity monitors, and body composition analysis.
- AI Recommendations: Tailored diet, movement, and lifestyle protocols for metabolic repair.
- Care Team & Lab Support: Continuous oversight by doctors, coaches, and nutritionists.
Outcomes:
- Clinical trials report over 70% diabetes remission.
- Weight reduction, improved heart markers, and energy levels.
- Strong evidence for reversing insulin resistance.
Positioning:
For people asking “Is diabetes reversal possible at a clinical, scientific level?”, Twin Health demonstrates that technology-driven precision care makes it achievable.
Freedom from Diabetes (FFD) – Dr. Pramod Tripathi
Background:
Since 2013, FFD has become one of India’s most recognized diabetes reversal movements, with tens of thousands of participants benefiting.
Philosophy:
FFD’s guiding principle: yes, diabetes reversal is possible if a person addresses all aspects of health — diet, exercise, stress, and mindset.
How It Works:
- Four Pillars: Low-glycemic nutrition, yoga and strength training, meditation & NLP, plus medical monitoring.
- Structured Programs: From discovery workshops to intensive 12-week journeys.
- Holistic Approach: Ayurveda, mindfulness, and behavioral therapy integrated with modern science.
- Community: Support groups, online sessions, and shared journeys.
Outcomes:
- 15,000+ participants have reduced or stopped medication.
- Reversal of related conditions like hypertension, fatty liver, and PCOS.
- Many sustain remission and improved quality of life.
Positioning:
Ideal for those seeking not just sugar control but a holistic lifestyle transformation proving diabetes reversal is possible.
Is Diabetes Reversal Possible? HealthyWayFit Shows You How

Living with diabetes often feels like carrying an invisible weight. You may be told to “eat less,” “exercise more,” or “try another pill.” And yet, your sugars stay stubborn, energy dips continue, and every lab report feels like a warning. So, many people wonder: is diabetes reversal possible?
The answer is yes — but not with quick fixes or generic advice. What’s missing isn’t willpower, it’s the right system. That’s where HealthyWayFit comes in.
We are not another app, generic webinar, or mass-market diet chart. HealthyWayFit is India’s most personal 12-month diabetes reversal program, designed exclusively for professionals who need a solution that works with their lifestyle.
Over the past few years, we’ve guided hundreds of Indians toward lowering HbA1c, reducing medicine dependency, and—in many cases—achieving complete reversal.
Our approach is simple: empathetic, therapeutic, and committed. We listen first, design second, and stay with you every step of the way.
1) What Makes HealthyWayFit Different?
Personalized Nutrition That Fits Your Life
No quinoa fads or smoothie charts. We work with your ghar ka khana — dal, roti, rice, idli, dosa, paneer, sabzi — and align it to your sugar control. No separate cooking, no pressure at home. A plan you can follow at 35 or 85.
Metabolic Exercise That Delivers Fast Results
Simple movements targeting big muscle groups (legs, shoulders, glutes) often bring sugar levels down by 50–100 points in just 15–20 minutes. No gym membership required.
Stress & Sleep Mastery
Stress spikes cortisol, which spikes sugar. We provide practical tools: one-minute breathing routines, sleep optimization, and micro-habits so your sugars remain stable even when life is busy.
Doctor-Led, Holistic Care
You’ll work directly with a Senior MD Diabetologist, ensuring medical safety while our coaches optimize lifestyle. This unique blend is why our clients see results others only promise.
Relentless Support & Accountability
Weekly coaching calls, daily check-ins, habit tracking, and special guides for festivals, dining out, travel, and weddings. Because life won’t stop for your health journey.
2) What Results Can You Expect?
Most clients notice changes in 20–60 days — better energy, lighter mornings, and lower sugar readings. Over the full program, we aim for stabilization and sustained reversal, not just short-term fixes.
3) Is HealthyWayFit for You?
If you’re a working professional or entrepreneur serious about taking control of your diabetes, and can dedicate just 15–30 minutes daily, then yes. This isn’t a crash course. It’s a proven system built around your food, family, and lifestyle.
4) Take the Next Step
If you’re asking “Is diabetes reversal possible for me?” — the first step is a personal consultation. We’ll review your health markers, lifestyle, and goals, then design a plan only for you.
Explore more at https://www.healthywayfit.com/
Book your consultation at Calendly
Because diabetes doesn’t just need to be managed. With the right system, it can be reversed — sustainably, safely, and with support at every step.
Frequently Asked Questions(FAQs)
1) Does genetic predisposition increase the likelihood of diabetes?
Yes, genetic predisposition significantly increases the likelihood of type 2 diabetes. If family members have diabetes, the risk is higher due to inherited insulin resistance or reduced beta cell function.
While lifestyle changes can delay onset, genetics make some individuals more vulnerable even with healthy habits.
2) Can diabetes be reversed permanently or only managed?
Diabetes reversal is possible, but usually considered remission rather than a permanent cure. Through weight loss, diet changes, and physical activity, blood sugar can return to normal ranges.
However, relapse is possible if healthy routines lapse. Long-term management is essential, as underlying risk factors remain.
3) Why are insulin levels important in controlling blood glucose?
Insulin regulates how the body uses and stores glucose. Balanced insulin levels move sugar from the bloodstream into cells for energy. When insulin is too low or the body resists its action, blood glucose rises, leading to diabetes. Monitoring insulin response is crucial for effective glycemic control.
4) How do beta cells function and what role do they play in diabetes?
Beta cells, located in the pancreas, produce insulin that controls blood glucose. In diabetes, these cells may fail to produce enough insulin or become overworked due to resistance. Their dysfunction is a central factor in both type 1 and type 2 diabetes, making them critical for disease management.
Conclusion
Diabetes is a complex condition shaped by genetics, lifestyle, and biological factors, but modern science shows that reversal is possible for many.
Programs in India like Sugarfit, Twin Health, and FFD, along with initiatives like HealthyWayFit, prove that structured lifestyle interventions, weight loss, and holistic care can move diabetic patients into remission.
While a complete cure remains elusive, sustained efforts—through balanced diets with healthy fats, exercise, and stress control—can restore blood sugar balance and improve long-term health.
Ultimately, diabetes doesn’t have to define one’s future; with the right system, support, and mindset, reversal is both achievable and sustainable.

.jpg)
