Managing diabetes mellitus goes far beyond diet changes alone. While nutrition plays an important role in blood sugar control, a comprehensive diabetes reversal program combines medical guidance, lifestyle strategies, and long-term support to create lasting results.
Many people struggle after a diabetes diagnosis, relying only on food adjustments or diabetes medications, but studies show that structured programs are more effective for reversing diabetes and improving overall health.
The best diabetes reversal program not only helps regulate blood sugar but also supports sustainable weight loss, improved body mass index, and reduced dependency on medication.
For women with gestational diabetes, these programs can also provide guidance for safe management during and after pregnancy.
By focusing on holistic changes instead of just diet, patients gain the tools to achieve lasting health benefits, including achieving weight loss and regaining energy—making these programs far more powerful than diet alone.
How Can You Choose The Best Diabetes Reversal Program For Long-Term Results?

Choosing the best diabetes reversal program means looking for more than quick fixes. A strong program focuses on long-term habits that can help you reverse diabetes, manage high blood sugar, and reduce future risks. Here are the key factors to consider:
1) Focus on Root Causes: Effective programs target insulin resistance, the main reason behind developing diabetes. By addressing how your body responds to insulin, you gain lasting improvements in disease control and overall health.
2) Nutrition That Works: Look for plans that prioritize healthy eating patterns rather than extreme restrictions. Balanced diets that include healthy fats, whole grains, and lean proteins are proven to stabilize blood sugar. According to the American Diabetes Association, sustainable nutrition is central to reversing diabetes safely.
3) Weight and Lifestyle Management : Carrying excess weight is one of the strongest risk factors for health complications. The right program should guide you through achievable lifestyle shifts that promote gradual weight reduction, improved energy, and better blood sugar balance.
4) Preventing Future Risks: Beyond short-term results, the best program prepares you to live without fear of developing diabetes again. With continuous support, you can maintain stable sugar levels, avoid complications, and enjoy lifelong health.
What Is Diabetes Mellitus And How Is It Different From Type 1 And Type 2 Diabetes?

Diabetes mellitus is a chronic condition where the body cannot properly regulate blood glucose and sugar levels, leading to serious long-term complications if left unmanaged. It occurs either because the body does not produce enough insulin or cannot use it effectively.
While lifestyle intervention, stress management, and balanced food intake are crucial for prevention and treatment, in severe cases, advanced options such as bariatric surgery may also be considered.
Without proper glycemic control, diabetes can lead to complications like kidney failure and heart disease.
Although they fall under the same category, Type 1, Type 2, and pre diabetes are different stages or forms of the disease:
- Type 1 Diabetes
- An autoimmune condition where the body destroys insulin-producing cells.
- Usually diagnosed in childhood or adolescence.
- Managed with insulin therapy and careful monitoring of sugar levels.
- Type 2 Diabetes
- Linked to food intake, excess weight, and poor lifestyle choices.
- Research suggests that lifestyle intervention, stress management, and reducing saturated fats in the diet significantly improve outcomes.
- Strongly associated with insulin resistance, making glycemic control essential.
- Pre Diabetes
- A warning stage where sugar levels are higher than normal but not yet Type 2.
- Research suggests that early lifestyle intervention such as healthy diet, exercise, and reduced saturated fats can prevent the progression.
- Regular monitoring and adjustments to food intake help maintain stability.
What Are The Best Ways To Manage Gestational Diabetes During Pregnancy?

Managing gestational diabetes during pregnancy is crucial for both the mother and the baby. With the right approach, you can keep diabetes under control, reduce high risk complications, and even lower your chances of developing Type 2 diabetes later.
1) Choose Whole Grains Over Refined Grains
- Limit refined grains such as white bread, white rice, and pasta that cause rapid spikes in blood sugar.
- Instead, add whole grains like oats, quinoa, and brown rice for better balance.
- Whole grains digest slowly, supporting stable sugar control and long-term diabetes management.
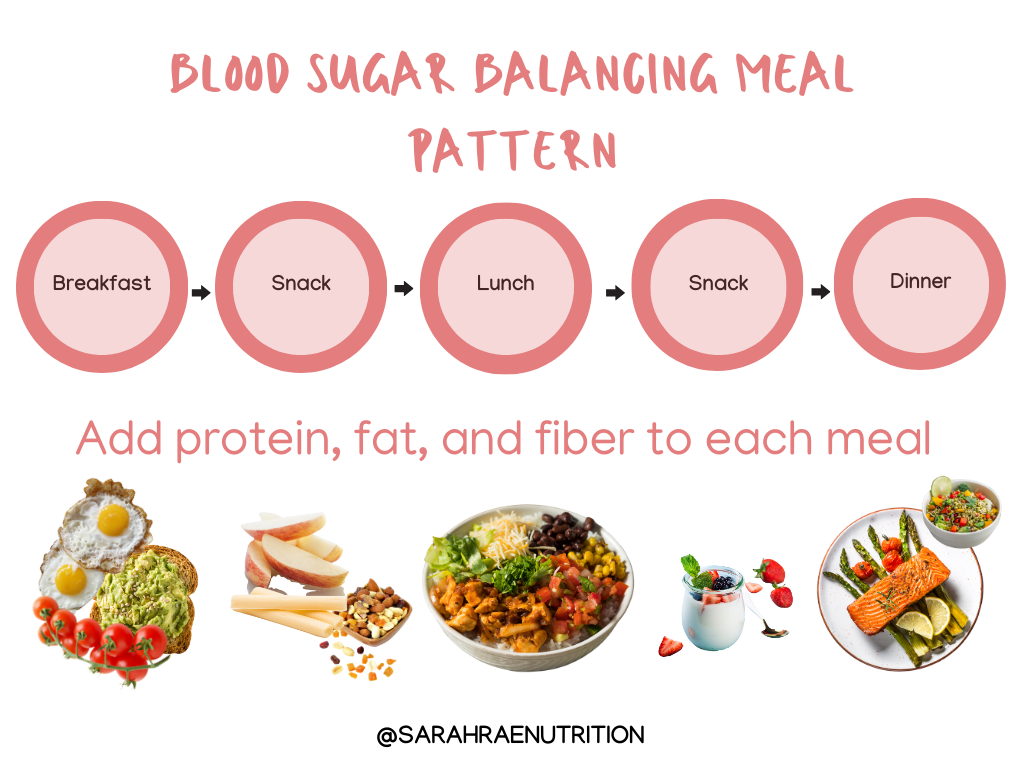
2) Eat Smaller Portions Frequently
- Instead of eating large meals, try to eat smaller portions throughout the day.
- This prevents sudden sugar spikes and helps keep energy levels steady.
- It’s especially important for pregnant women at high risk of blood sugar fluctuations.
3) Make Healthy Lifestyle Adjustments
- Combine nutritious food intake with moderate activity such as walking or prenatal yoga.
- These lifestyle adjustments improve insulin sensitivity and help regulate sugar naturally.
- They also reduce the chances of developing future diabetes.
4) Prevent Diabetes After Pregnancy
- Many women experience complete remission of gestational diabetes after childbirth.
- However, sticking to healthy eating patterns with whole grains, lean proteins, and vegetables can help prevent diabetes in the future.
- Ongoing follow-ups with doctors ensure better disease control and reduce the risk of long-term complications.
What Are The Best Healthy Eating Habits For Controlling Blood Sugar?
Managing blood sugar isn’t just about medication—it’s about adopting a balanced diet, making smart lifestyle changes, and pairing them with regular physical activity. Good nutrition helps lower the risk of complications like vision loss and heart attacks, while also being more cost effective in the long run.
1) Focus on a Balanced Diet
- A healthy diet should include fiber-rich foods such as vegetables, legumes, and whole grains.
- These foods slow digestion, prevent sugar spikes, and improve overall blood sugar stability.
- Consistency in meal planning is as important as what you eat.
2) Limit Added Sugars and Refined Foods
- Avoid foods high in added sugars such as sodas, candies, and processed snacks.
- These trigger rapid increases in blood sugar and can worsen insulin resistance.
- Replacing them with natural alternatives is a simple but powerful lifestyle change.
3) Eat in Smaller, Frequent Portions
- Instead of large meals of shorter duration, spread your diet into 4–5 smaller meals.
- This prevents spikes and crashes in blood sugar, keeping energy steady throughout the day.
- Such patterns have shown effectiveness in improving long-term glucose control.
4) Pair Diet with Physical Activity
- Combining a nutritious diet with regular physical activity is one of the most effective strategies for controlling blood sugar.
- Exercise enhances insulin sensitivity and supports weight management.
- Even moderate activities like walking can make a big difference.
5) Commit to Long-Term Lifestyle Changes
- Sustainable lifestyle changes like reducing refined carbs, choosing lean proteins, and mindful portion control are key.
- They not only regulate blood sugar but also lower the chances of serious complications such as heart attacks or vision loss.
- The best part? These methods are natural, safe, and cost effective compared to long-term medical treatments.
How Can You Lower High Blood Sugar Quickly And Safely At Home?

Important safety first — if you feel faint, are vomiting, breathing fast, confused, or have very high glucose with ketones, get urgent medical help (see “When to seek emergency care” at the end).
Below is a detailed, practical, evidence-based guide you can use at home to try to lower high blood sugar safely — with what to do first, what to avoid, and when to call your care team.
I’m not a doctor; follow your personal diabetes plan and contact your provider for advice specific to your medicines and situation.
1) Immediate checks (first 0–30 minutes)
- Re-test your blood sugar to confirm the reading (meters can misread).
- If your meter reads >240 mg/dL (13.3 mmol/L), check urine or blood ketones if you have the supplies. If ketones are present, do not exercise and contact your diabetes team — ketones with high glucose can signal diabetic ketoacidosis (DKA).
2) Quick actions you can safely try (if ketones negative and you feel well)
These are low-risk, home measures shown to help reduce blood glucose promptly.
a) Hydrate — drink plain water
- Drinking water helps replace fluids lost through urination and can help dilute blood glucose and support kidney clearance. Start with a large glass (250–500 ml) and sip regularly. In severe dehydration or vomiting seek medical care.
b) Do increased physical activity if safe (brisk walk or similar)
- A 10–30 minute brisk walk after checking ketones and confirming you’re well can lower blood glucose quickly by increasing muscle glucose uptake.
- Physical activity can also improve insulin sensitivity for many hours afterwards. Do NOT exercise if you have moderate/large ketones or feel unwell.
c) Take your prescribed medication exactly as advised
- If you use a correction insulin or a pre-agreed “sliding scale,” follow that plan. If you only take oral diabetes medicines, continue them as prescribed.
- Do not add extra doses or change insulin dose unless you have been instructed by your clinician — contact them if you think a dose change is needed.
d) Avoid high-carb and sugary foods
- Do not eat sugary snacks or drinks to “test” whether sugar will fall — that will raise levels. Instead, if hungry, choose low-carb, lean protein or non-starchy vegetables while you bring glucose down.
3) Foods, fats and why meal choices matter now
- Fats do not convert directly to glucose, but high-fat meals can produce delayed and prolonged high blood sugar later and may worsen insulin resistance; they’re not a good “fix” if you need to lower an acute spike.
- Prefer light, low-GI choices (non-starchy veg, lean protein) until glucose is controlled.
4) Monitoring after taking action
- Re-check your blood sugar in about 15–60 minutes after a walk or taking medication (or as your diabetes plan instructs).
- If levels are falling, continue the plan (hydrate, light activity, monitor). If levels stay the same or rise, contact your diabetes care team — you may need medication adjustment or medical review.
5) If you’re ill or cannot eat/drink
- Follow your “sick-day rules”: keep taking insulin/diabetes medication as advised, check glucose and ketones more frequently, stay hydrated, and call your care team earlier than usual. Illness commonly raises blood glucose and increases the risk of DKA.
6) When to call your clinician or go to emergency
Seek urgent medical attention (call emergency services) if any of the following apply:
- You have large/positive ketones, or blood ketone >1.6 mmol/L (or urine 2+), or symptoms of DKA (nausea/vomiting, abdominal pain, breathlessness, confusion).
- Blood glucose remains very high (e.g., >300 mg/dL) despite following the above measures and taking prescribed medication.
- You are vomiting and cannot keep fluids down, are drowsy, or breathing rapidly — go to the emergency room.
7) Practical “quick action” checklist (copyable)
- Confirm meter reading.
- If >240 mg/dL → check ketones.
- If ketones positive → DON’T exercise, call your clinician/ER.
- Drink water (250–500 ml).
- If ketones negative and you feel well → take a brisk 10–30 min walk (or similar increased physical activity).
- Take prescribed medication as directed (follow your correction plan if you have one).
- Re-test in 15–60 minutes. Repeat steps or call your team if levels do not come down.
8) Longer-term steps to prevent repeat spikes
Work with your team on medication optimization, portion control, choosing low-GI foods, regular physical activity, and weight management — these reduce the frequency of high readings and overall diabetes complications.
Can Stress Cause You To Develop Diabetes Over Time?
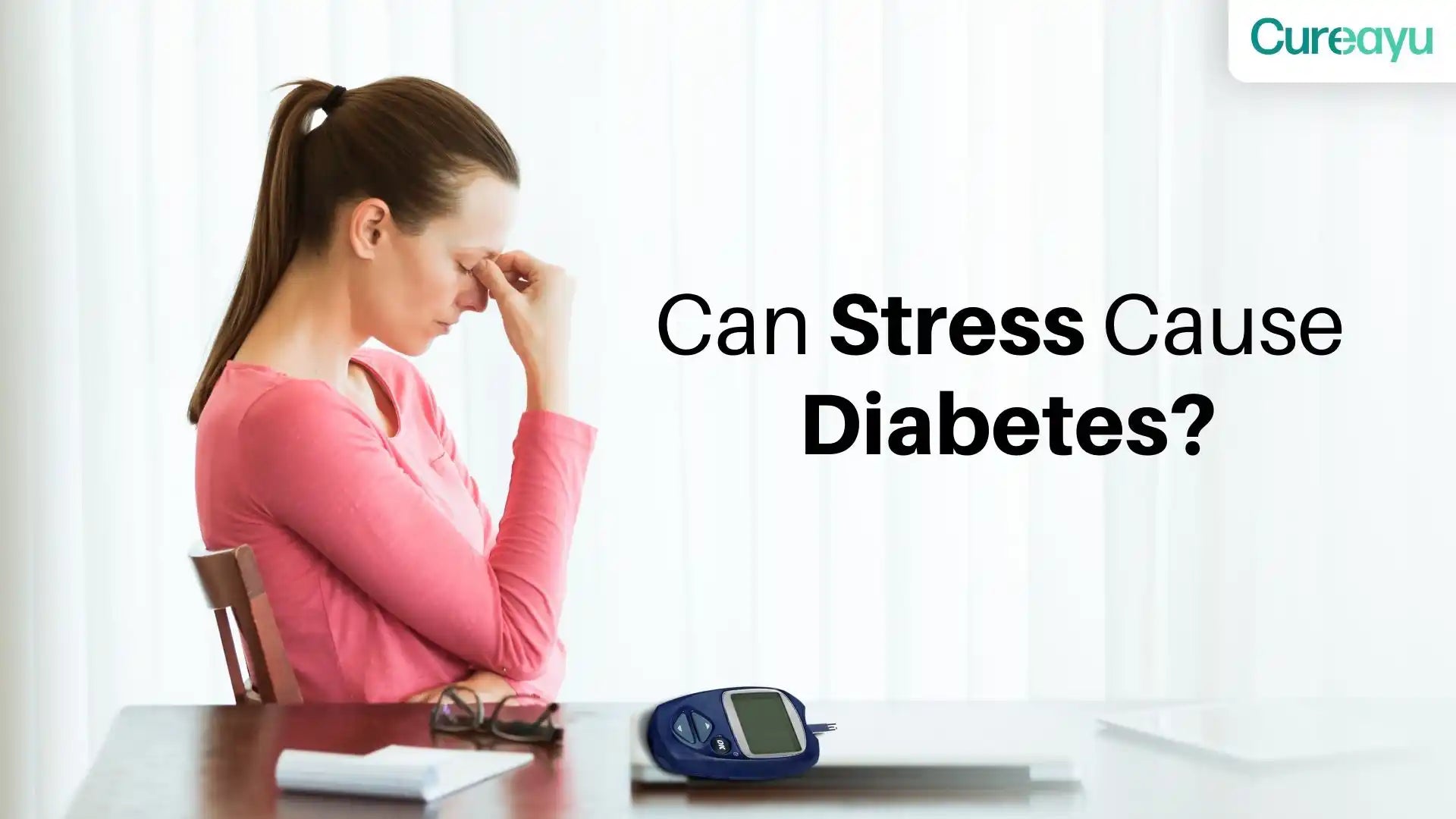
Yes — chronic psychological stress can raise your long-term risk of developing type 2 diabetes, but it’s not a single cause.
Stress works through biological pathways (hormones + inflammation), behavioural pathways (poor diet, less activity, poor sleep, weight gain), and can interact with certain medications to raise risk.
Many people under stress never get diabetes — risk depends on genetics, weight, lifestyle and medical care — but research shows stress is a meaningful contributor you can act on.
1) How stress affects the body (the biology — in detail)
- Stress hormones raise blood glucose. When you’re stressed your hypothalamic–pituitary–adrenal (HPA) axis and sympathetic nervous system release cortisol and catecholamines (adrenaline/noradrenaline).
- These hormones increase liver glucose production and reduce peripheral glucose uptake, so blood glucose and the insulin requirement go up. Repeated exposure to high cortisol promotes insulin resistance, a key step on the path to diabetes.
- Chronic stress → inflammation & oxidative stress. Long-term stress is linked with low-grade inflammation and oxidative stress that damage insulin signalling and beta-cell function over time.
- That biochemical damage helps explain how stress can contribute to the metabolic changes seen in diabetes.
2) What the research says (epidemiology & clinical studies)
- Prospective studies and reviews find an association.
- Several cohort studies and reviews report that people with sustained high perceived stress have higher odds of developing type 2 diabetes over years (effects vary by study and sex, and mediators like BMI and activity explain part — but not all — of the link).
- In one influential analysis moderate/high stress predicted higher diabetes risk within a few years.
- Stress speeds progression from prediabetes. Studies show higher perceived stress correlates with worse glycaemic measures (higher HbA1c) in people with prediabetes, and psychological distress is associated with faster progression to diabetes in some recent cohort data.
- That means stress can turn a warning stage (prediabetes) into full diabetes faster.
3) Behavioural / life pathways (how stress changes daily life)
- Comfort eating and poorer food choices. Stress commonly pushes people toward energy-dense, sugary, processed foods.
- Over time this raises calorie intake and central fat — both strong drivers of insulin resistance. (Good news: replacing processed snacks with whole foods and fruits helps — whole fruit is associated with lower diabetes risk while fruit juice often does not share that benefit.)
- Less physical activity & worse sleep. Chronic stress reduces motivation to exercise and disrupts sleep; both of these make insulin resistance and weight gain more likely.
- Substance use and medicine adherence. People under stress may drink more alcohol, smoke, or skip preventive medical visits / medicines — each of these increases diabetes risk.
4) When “medications” and stress interact
- Glucocorticoids (steroids) — used for many inflammatory conditions — reliably raise blood sugar and can cause new-onset steroid-induced diabetes or unmask prediabetes.
- The effect is dose- and duration-dependent and may resolve when steroids stop, but not always. If you’re prescribed steroids, glucose should be monitored and managed with your clinician.
- Some psychiatric medicines (particularly some atypical antipsychotics) are linked to weight gain, insulin resistance and higher diabetes risk. If you’re taking such medicines, the metabolic side-effects should be discussed with your doctor and monitored regularly.
5) Practical, evidence-based ways to reduce stress-related diabetes risk
(These work biologically and by improving your everyday life.)
A. Stress-management techniques (research-backed)
- Mindfulness / MBSR, CBT, relaxation training — randomized trials and meta-analyses show these can reduce stress, diabetes distress and in many studies improve HbA1c modestly when added to usual care. Incorporate short daily practices (10–20 min) or structured programs if possible.
B. Diet & food choices
- Prioritise a balanced diet rich in vegetables, whole grains and whole fruits (not fruit juice). Whole-fruit intake is associated with lower diabetes risk in cohort studies and meta-analyses. Watch portion sizes and limit added sugars and processed snacks.
C. Move more in daily life
- Regular physical activity improves insulin sensitivity and buffers stress responses. Aim for routine aerobic exercise plus resistance work — even brisk walking 30 min most days helps.
D. Sleep and routines
- Fixing sleep (regular bedtimes, sleep hygiene) reduces stress hormones and improves glucose metabolism.
E. Medical follow-up
- If you have prediabetes or high risk, get periodic glucose checks (fasting glucose, HbA1c). For some high-risk people, medicine such as metformin is used to delay progression — discuss this with your clinician.
- Yale Medicine and diabetes prevention programs highlight that diet, exercise and sometimes medication together lower progression risk.
6) What to expect — realistic, research-grounded perspective
- Stress is a modifiable risk factor but not the only one. Research shows stress explains part of the risk, but BMI, activity, diet, genetics and medications explain much of the remaining risk.
- Reducing stress reduces both the biological burden and the unhealthy life-habits that build up over years, so it’s a valuable prevention target.
7) Quick checklist (actions you can take this week)
- Get a baseline check (fasting glucose/HbA1c) if you have risk factors or prolonged stress.
- Add 10–20 minutes daily of a stress practice (mindfulness, breathing, short walk).
- Swap sugary snacks for whole fruits and fibre-rich foods.
- Aim for regular physical activity and 7–9 hours sleep per night.
- If you take steroids or antipsychotics, ask your prescriber about glucose monitoring and metabolic checks.
Diabetes Reversal Programs in India: Brand Profiles
Sugarfit
Background:
Founded in 2021 in Bengaluru, Sugarfit is a health-tech startup focused on type 2 diabetes and pre-diabetes reversal. The platform emphasizes technology-driven lifestyle interventions over long-term medication. sugarfit
Philosophy:
Sugarfit promotes personalized, preventive, and data-driven diabetes management, using real-time health data to guide lifestyle changes.
Features & Approach:
- Continuous Glucose Monitoring (CGM): Tracks daily glucose variations.
- Medical Oversight: Regular doctor consultations and medication adjustments.
- Personalized Nutrition & Fitness: Diet plans and exercise routines tailored to glucose patterns.
- Stress & Mindfulness: Breathing exercises, meditation, and behavioral coaching.
- Lab Tests & Community Support: Periodic screenings and live online classes for motivation.
Outcomes:
- Participants with high HbA1c (>9) see ~20% reduction in 90 days.
- Many reduce or stop medications.
- Improved energy, sleep, and weight management reported.
Positioning:
Ideal for urban, digitally literate patients seeking structured, tech-enabled diabetes care with measurable progress.
Twin Health
Background:
Twin Health, founded in Silicon Valley, offers the Whole Body Digital Twin™ (WBDT™), an AI-driven system for metabolic health. Now available in India via hospitals and corporate programs. twinhealth
Philosophy:
Chronic conditions like diabetes result from systemic imbalances. Twin Health uses precision medicine to address root causes instead of only managing symptoms.
Features & Approach:
- Whole Body Digital Twin™: AI-based personalized metabolic model.
- Wearables & Tracking: CGM, fitness devices, and body composition data.
- AI Recommendations & Multi-Phase Program: Diet, exercise, and lifestyle tailored to improve metabolism and organ health.
- Care Team & Lab Monitoring: Doctors, coaches, and nutritionists with continuous evaluation.
Outcomes:
- Over 70% remission reported in clinical trials.
- Weight reduction, improved cardiovascular markers, and enhanced energy.
- Effective reversal of insulin resistance.
Positioning:
Best for individuals seeking technology-intensive, clinically validated diabetes solutions backed by AI and advanced diagnostics.
Freedom from Diabetes (FFD) – Dr. Pramod Tripathi
Background:
Founded in 2013, FFD is one of India’s leading lifestyle-based diabetes reversal programs, helping tens of thousands reduce or eliminate medication dependence. freedomfromdiabetes
Philosophy:
FFD emphasizes a holistic approach, combining diet, exercise, stress management, and emotional well-being, blending modern science with Indian wellness practices.
Features & Approach:
- Four Pillars: Nutrition (low-glycemic diet), Exercise (yoga & strength training), Inner Transformation (meditation & NLP), Medical Monitoring.
- Structured programs: From discovery sessions to 12-week intensive programs.
- Holistic practices: Ayurveda, mindfulness, behavioral therapy.
- Community support and online accessibility.
Outcomes:
- 15,000+ participants have reduced or stopped medications.
- Reversal of conditions like hypertension, fatty liver, and PCOS.
- Long-term remission and improved quality of life.
Positioning:
Appeals to those seeking a holistic, community-driven, lifestyle-first approach to diabetes management.
HealthyWayFit — India’s Best Diabetes Reversal Program

Living with diabetes often feels like carrying an invisible weight. You’re told to “eat less,” “exercise more,” or “try another pill.” And yet, your sugars stay stubborn, energy dips continue, and every lab report feels like a warning. What’s missing isn’t willpower — it’s the right system.
That’s where HealthyWayFit comes in — the best diabetes reversal program in India, built for real people with real lives.
We are not another app, generic webinar, or mass-market diet chart. HealthyWayFit is a 12-month, end-to-end diabetes reversal program designed exclusively for Indian professionals who need a solution that fits seamlessly into their lifestyle.
Over the past few years, our team has guided hundreds of Indians toward lowering HbA1c, reducing medicine dependency, and — in many cases — achieving complete reversal.
Our tone is simple: empathetic, therapeutic, and committed. We listen first, design second, and stay with you every step of the way.
1) What Makes HealthyWayFit the Best Diabetes Reversal Program?
1. Personalized Nutrition You Can Actually Live With
No quinoa fads or complicated smoothie charts. We work with your ghar ka khana — dal, roti, rice, idli, dosa, paneer, sabzi — and align it to your sugar control. No separate cooking, no pressure at home. A plan you can follow at 35 or 85.
2. Metabolic Exercise That Works Fast
We introduce simple metabolic movements targeting big muscle groups (legs, shoulders, glutes). These routines, which take just 15–20 minutes, often bring sugar levels down by 50–100 points. No gym membership required.
3. Stress & Sleep Mastery
Work deadlines, family responsibilities, or city traffic — stress spikes cortisol, which in turn spikes sugar. We give you practical tools: one-minute breathing routines, sleep optimization, and micro-habits to keep your sugars stable even when life is busy.
4. Doctor-Led, Holistic Care
You’ll work directly with a Senior MD Diabetologist who monitors your medical safety while our coaches optimize lifestyle. This unique blend of medical oversight and lifestyle expertise is why our clients see results others only promise.
5. Relentless Support & Accountability
Weekly coaching calls, daily check-ins, habit tracking, and even festival, dining-out, travel, and wedding guides. Life won’t stop for your health journey — and that’s why HealthyWayFit adapts with you.
2) What Results Can You Expect?
Most clients begin to see noticeable changes in just 20–60 days, whether that’s improved energy, lighter mornings, or lower sugar readings. Over the full program, we aim for stabilization so results are not just temporary but sustainable year after year.
This is what makes HealthyWayFit stand out as the best diabetes reversal program — it’s not just about quick fixes, it’s about long-term transformation.
3) Is HealthyWayFit Right for You?
If you are a working professional or entrepreneur who is serious about taking control of your diabetes, and if you can dedicate just 15–30 minutes a day to your health, HealthyWayFit is built for you. This isn’t a crash course. It’s a life-changing system, personalized around your food, family, and lifestyle.
4) Take the Next Step
The journey begins with a personal consultation where we understand your current challenges, health markers, and lifestyle. If we’re aligned, we’ll design a custom plan tailored only for you.
Visit HealthyWayFit to explore how the best diabetes reversal program in India can help you move beyond “managing” diabetes and actually reverse it — sustainably, safely, and with support at every step.
Book your appointment for a consultation directly on Calendly and take the first step today.
Frequently Asked Questions(FAQs)

1) What is insulin resistance and how does it lead to type 2 diabetes?
Insulin resistance occurs when the body’s cells respond poorly to insulin, forcing the pancreas to produce more. Over time, this strain exhausts beta cells, raising blood glucose.
Persistently high sugar levels, combined with reduced insulin effectiveness, eventually progress to type 2 diabetes, increasing risk for long-term complications.
2) What lifestyle modifications are most effective for managing diabetes?
The most effective lifestyle modifications include adopting a balanced diet rich in whole grains, vegetables, and lean proteins, regular physical activity, weight management, stress reduction, and adequate sleep.
Together, these measures improve insulin sensitivity, stabilize blood sugar, reduce dependence on medication, and lower the risk of diabetes complications.
3) What are the risks and benefits of bariatric surgery for diabetes management?
Benefits: Bariatric surgery often results in significant weight loss, improved insulin sensitivity, remission of type 2 diabetes, and reduced cardiovascular risk.
Risks: Possible complications include nutrient deficiencies, infection, and surgical risks. Lifelong dietary adjustments and medical follow-ups are required, but overall, it can be life-changing for severely obese patients.
4) What types of physical activity are best for diabetes control?
For diabetes control, a mix of aerobic exercises (like walking, cycling, or swimming) and resistance training (like weights or bodyweight workouts) is most effective.
Aerobic activity improves insulin sensitivity, while strength training increases muscle mass, helping the body utilize glucose better. Flexibility and balance exercises also enhance overall health.
5) What lifestyle changes can help prevent the onset of diabetes?
Key changes include maintaining a healthy weight, adopting a balanced diet low in refined sugars, engaging in regular physical activity, managing stress, and ensuring quality sleep. Avoiding smoking and limiting alcohol also reduce risk.
These steps collectively improve insulin function, regulate blood sugar, and prevent diabetes progression from prediabetes.
Conclusion
Diabetes management and reversal require more than diet alone — it’s about addressing the root causes like insulin resistance with a holistic, long-term approach.
The best diabetes reversal programs integrate personalized nutrition, metabolic exercise, stress management, and medical oversight, offering sustainable results beyond temporary fixes.
While bariatric surgery helps some patients, lifestyle modifications such as balanced eating, regular activity, weight management, and stress reduction remain the safest and most effective foundation.
By adopting these changes early, people can not only control but often reverse type 2 diabetes, prevent complications, and achieve lasting improvements in overall health and energy.

.jpg)
